
 From Patient to advocate: how self tracking is empowering parkinson's patients
From Patient to advocate: how self tracking is empowering parkinson's patients
If you're reading this, you may be someone with Parkinson's disease (PwP), or you may know someone who has it. We won't bore you the usual information about the condition since you likely already know it. While Parkinson's is incurable, it doesn't necessarily shorten one's lifespan. Many people live 20-30 years with it. As Sara Riggare points out in an article, "We have to know why we do what we do" as a patient or caregiver. Adopting this perspective is the first step in the "From Patient to Advocate" collection.
In this blog post, we'll discuss how Parkinson's patients change their traditional role by self-tracking and working together for better care. Also, we encourage you to see yourself as people with Parkinson's, not just as a patient. Remember that Parkinson's is only one part of your life, and you can manage it.
From Passive to Proactive: The Changing Role of PwP in Healthcare
The traditional role of Parkinson's disease (PD) patients as passive recipients of healthcare advice is significantly transforming. With the advent of technology and self-tracking tools, people with Parkinson’s are embracing an empowered role in their care. Patients are no longer content to follow advice unthinkingly, becoming active participants in decision-making, sparking a positive shift in the dynamics of PD management.
The primitive benefit of self-tracking for people with Parkinson's is that monitoring and tracking create a sense of empowerment. It allows them to shift from passive care recipients to active participants in their well-being. This increased sense of control can boost their confidence and positively impact their emotional well-being. Additionally, self-tracking enables individuals to take ownership of their health journey, leading to a greater sense of self-efficacy and overall satisfaction with their care. It empowers individuals to actively participate in their well-being and treatment decisions and promotes a stronger patient-provider relationship.
Why I self-track, How and what I self-track, Lessons learned from self-tracking
In one clinical study (Riggare et al.), named “You have to know why you're doing this: a mixed methods study of the benefits and burdens of self-tracking in Parkinson's disease,” researchers asked 180 patients why they were self-tracking:
The respondents in the interviews mentioned various reasons for engaging in self-tracking. Here are some key motivations they shared:
Mindset for self-tracking: Some individuals expressed having a natural inclination or attitude. They were inherently interested in monitoring their health, tracking symptoms, and gathering data related to their Parkinson's disease (PD). This mindset likely contributed to their engagement and commitment to self-tracking activities.
The individuality of PD: The respondents demonstrated an understanding of the highly individualised nature of PD. They recognised that the presentation and progression of the disease can vary significantly from person to person. In light of this, they emphasised the importance of understanding their unique symptoms and finding personalised strategies to manage them effectively.
“I expect tracking to help me more clearly see how my disease is; now it’s mostly guesswork.”
Increased awareness: Self-tracking was described as enhancing awareness of their illness and its progression. By actively monitoring their symptoms, treatment responses, and lifestyle factors, individuals could better understand how PD impacts their daily lives. This heightened awareness allowed them to make informed decisions about self-care, treatment adjustments, and lifestyle modifications.
“It’s important to take your medication right, at the right time. You can get a bad effect; it doesn’t always mean you need to increase your dose; it can mean you need to make it more evenly distributed.”
In the same study, researchers asked patients how and what they self-track.
The number one thing people tracked was their medication: when they took it and how often. This helps them take their medications at the best times. Other crucial factors they followed included stress levels, diet, and sleep. Understanding these elements of health and how they interact is critical to getting the most out of self-tracking.
One experienced participant in the study pointed out the challenge of tracking more subjective health measures, like what it means to them to "feel well."
“It was tough work to constantly think about whether I didn’t feel pain somewhere, if I didn’t feel stiff and so on… It took over my life... So I realised that I have to register something else, and I decided to note when I am doing well instead of when my symptoms are on the level I want them to be.”
When it comes to the tools used for tracking, technology plays a significant role. Many participants used activity trackers, smartphone apps for sleep and exercise, and spreadsheet programs to gather and visualise their data. But only some things were high-tech. Surprisingly, participants used good old-fashioned pen and paper even more, and many kept track in their minds.
Use It or Lose It: It’s Never Too Late to Get Moving in Parkinson’s
The study showed that, Interestingly, the tracking mode didn't seem to relate to factors like age, gender, or education level. Specifically, the study revealed that people diagnosed with PD for more than five years were likelier to use pen and paper as their preferred tracking method. This suggests that the duration of PD may influence the choice of tracking mode, with people who have had the condition for a longer time being more inclined to use traditional pen and paper methods for tracking.
Overall, the motivations for self-tracking expressed by the respondents revolved around a proactive mindset, recognising the individuality of PD, and seeking increased awareness of their condition. By engaging in self-tracking, they aimed to gather personalised data, monitor their symptoms, and gain insights into the progression of their illness. These motivations reflect a desire for self-empowerment, better self-management, and a deeper understanding of their health experiences.
Self-tracking in Parkinson’s: The lived efforts of self-management
In the study (Vafeiadou et al.), "Self-tracking in Parkinson's: The lived efforts of self-management," researchers examined online members' discussions about self-monitoring about performing Parkinson's self-management. The 5,000 post-data corpus obtained from HU were analysed using qualitative data software. The results show that PwP tracked information in four main categories: treatment, Parkinson's symptoms, general health indicators, and lifestyle.
Self-tracking practices from this study.
One PwP reported tracking treatment across a period to reach an optimal level of medication dosage:
“Started wearing off in March 2013 after 1.5 hours. Neuro seems stumped, so I have started experimenting. For some reason, my mornings are still OK - better than off-time. So now I start at noon, 1x100 Sinemet, then 1x100 every hour until 8 pm, no off-time, can go 1 hr 15 min but no more. It concerns me that this may be too much for me (from 450 to 900 mg). I have tried 200 mg – no difference. It seems that it’s all about experimenting till you find the right döşe; it seems no doc can predict that but may be able to keep you out of trouble.”
As one PwP explained, not only did tracking lifestyle information help to support a healthy routine for self-management but it was also used to assess the achievement of initial goal setting:
“Exercise exercise exercise must move as much as possible best medicine. Try and keep a workout diary and plan your next day or week. Give yourself goals to Meet. This will help you stay motivated and focused.”
One of the PwP explained that familiarity with phones generated a sense of control over self-tracking:
“Very relaxing, the phone gives you full control. Nothing to adjust or think about. Press the start button in the morning when you take the medicine.” Another criterion was flexibility, with tools capturing information that could concurrently support multiple goals perceived as applicable: “I’ve got two charts going now. One is hourly to record my motor fluctuation, and one is daily to record other symptoms, exercise, etc. I have these on my laptop.”
A sensemaking approach to Parkinson’s Disease from Self-tracking
Sensemaking is a cognitive process crucial in informing health-related actions and reflecting individuals' efforts to make sense of their health. In Parkinson's disease (PD), sensemaking refers to how individuals interpret and understand their condition, symptoms, and the impact on their overall well-being. It involves actively seeking meaning, making connections, and creating a coherent understanding of their health experiences. The sensemaking framework proposes that individuals perform chronic health self-management activities in the habitual and sensemaking modes. Each mode includes three interdependent processes: perception, inference, and action. (Mamykina et al.)
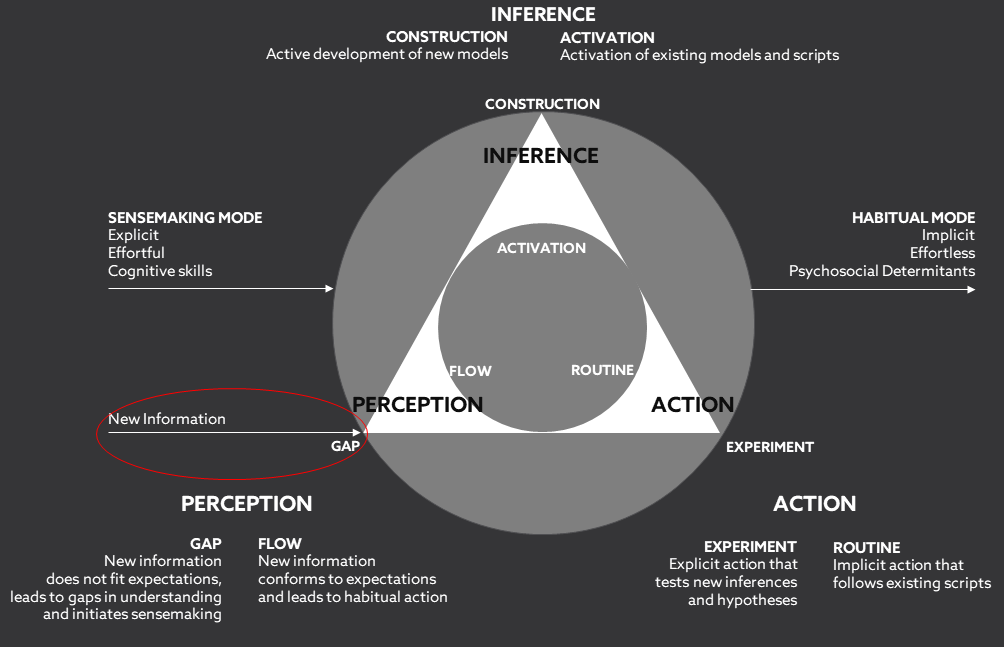
Sensemaking framework for chronic disease self-management, adopted from Mamykina et al.
Habitual mode
When in the habitual mode, PwP perceived new information, after which their existing mental models were activated to make appropriate inferences. The following quote illustrates a belief in the regular manner relating to the onset of tremor (Adopted from Vafeiadou et al.):
“My tremor usually worsens during the day until it is almost continuous during the evening. I often find that even if I don’t have a tremor at tablet time, I develop one soon after taking the meds.” In a similar example, a different PwP had constructed a routine activity carried out when their well-being was at its best:
In a similar example, a different PwP had constructed a routine activity carried out when their well-being was at its best:
“Morning is generally good for me, so I usually plan my exercises and physical activities during that time”.
Sensemaking mode
As the sensemaking framework predicts, the sensemaking mode was triggered when PwP perceived new information from self-tracking collected over a timespan, which could not be explained by previous experiences or general knowledge. Examples of this included periods of medication efficiency and suddenly disrupted symptoms. The following illustrative quote comes from a PwP who adhered to a daily medication schedule and tracked the response to medication over time. This led them to identify a timeframe in the day during which the drug didn’t work as expected, combined with an unexplained negative impact on mood. This new information could not be reconciled with the existing mental model of how this medication worked, triggering the person’s sensemaking mode due to a gap in disease understanding. (Adopted from Vafeiadou et al.):
“Why the same time every day? Why do I fall apart at the same time every day? Almost every day, I get depressed, and my meds don’t work or work poorly. It was at night, about 5 or 7 pm, but it has moved to mid-afternoon. I still take my meds at the same time as always. It will last for an hour or 2.”
Finally, the action phase of sensemaking!
Finally, PwP proceeded to the action phase of sensemaking by testing their new inferences. This was achieved by engaging in active experimentation to evaluate the impact of their different choices. In the following example, a PwP reported on a treatment experiment with Mucuna pruriens, i.e., a tropical legume used by PwP as an alternative supplement to traditional drugs. (Adopted from Vafeiadou et al.):
“I’ve taken MP with water, juice, and hot pineapple juice as a hot beverage. That last worked pretty well. I’m currently testing taking MC when I first begin sensing chest fasciculations, letting me know the C/L is running out with a cup of black tea. After a few minutes, it kicks in then I find I can put off taking the C/L until a little warmth, not hyperpyrexia, begins. I don’t think it needs to be this complicated, and I’m seeking something simple that has eluded me so far.”
A PwP explained how they tracked his blood pressure concerning his Parkinson’s medication regime. PwP aimed to understand if his doctors’ diagnosis of hypertension was correct or if the elevated blood pressure resulted from their Parkinson’s medication.
“My doctors all wanted me to get back on one of the blood pressure meds, but I was sure my problem wasn't hypertension but was triggered by levodopa issues. I was proved right…The point here is that in the nearly two years that I was closely monitoring my bp, I saw a definite linkage between the BP readings and the levodopa in my system – – low readings midway between pills, readings going up as we approached the time for a new pill, peaking at pill time, and going down as the new pill took effect.”
Personalised treatment from self-tracking
Self-tracking data can facilitate discussions between patients and healthcare providers, enabling more personalised treatment decisions. It can help identify patterns, triggers, and potential correlations between different factors and symptoms. For example, tracking medication intake and symptom fluctuations may reveal optimal dosing schedules or adjustments. Monitoring exercise routines and their impact on symptom management may provide insights into the effectiveness of specific activities.
However, it's important to note that self-tracking should complement professional medical guidance rather than replace it. The data collected through self-tracking should be shared and discussed with healthcare providers to ensure accurate interpretation and appropriate adjustments to treatment plans. Personalised treatment approaches should be developed in collaboration with healthcare professionals with expertise in Parkinson's disease management.
Current technology for self-tracking
Wearable devices such as smartwatches can continuously monitor various aspects of an individual's movement. In the context of Parkinson's disease, smartwatches can provide objective measurements of motor symptoms, including tremors and dyskinesia (involuntary movements). They can track parameters such as step count, offering insights into an individual's mobility and physical functioning throughout the day.
Breaking barriers: Assessment of the moment
Parky, an FDA-cleared digital buddy, is here to revolutionize how you manage Parkinson's disease (PD). Wave goodbye to uncertainty! With Parky, you can actively track your motor symptoms, stick to your medication schedule and promote physical activity while improving access to care.
Think of Parky as your health diary, always there to help you self-track and self-monitor your PD conditions. You're not alone on this journey, and Parky will ensure you, your caregivers, and your loved ones can make the best decisions for your health.
What makes Parky so unique? First, PD symptoms can change daily, and everyone's experience is different. But with Parky's self-tracking technology, you can monitor your symptoms and see how further lifestyle changes might impact them.
Join our community in spreading hope and strength. Tell us your unique journey with Parkinson's to uplift and empower others.